- Do You Pay Copay For Annual Physical
- Copay For Annual Physical Exam
- Medicare Pay For Annual Physical
- Copay For Annual Physical Record
- Copay For Annual Physical Appointment
Do You Pay Copay For Annual Physical
A copay is like paying for repairs when something goes wrong. When your car gets serviced, you pay a set fee to the mechanic, just as you may pay a set fee, like $20, when you go to the doctor because you're sick. Every plan is different, so premiums, deductibles, coinsurance, and copays can vary in cost. Health care question answered. There’s no coinsurance, copay or deductible for an annual wellness visit. If the member has had Medicare Part B for more than 12 months, they’re entitled to an annual wellness visit with a primary care provider to develop or update a personalized prevention plan, based on.
The following tables provide examples of cost-shares or copayments and annual deductibles for families who use civilian providers and facilities under each of the three Tricare options.
When Beverly Dunn called her new primary care doctor’s office last November to schedule an annual checkup, she assumed her Medicare coverage would pick up most of the tab.
The appointment seemed like a routine physical, and she was pleased that the doctor spent a lot of time with her.
Until she got the bill: $400.
Dunn, 69, called the doctor’s office assuming there was a billing error. But it was no mistake, she was told. Medicare does not cover an annual physical exam.
Dunn, of Austin, Texas, was tripped up by Medicare’s confusing coverage rules. Federal law prohibits the health care program from paying for annual physicals, and patients who get them may be on the hook for the entire amount. But beneficiaries pay nothing for an “annual wellness visit,” which the program covers in full as a preventive service.
“It’s very important that someone, when they call to make an appointment, uses those magic words, ‘annual wellness visit,’” said Leslie Fried, senior director of the Center for Benefits Access at the National Council on Aging. Otherwise, “people think they are making an appointment for an annual wellness visit and it ends up they are having a complete physical.”
Email Sign-Up
An annual physical typically involves an exam by a doctor along with bloodwork or other tests. The annual wellness visit generally doesn’t include a physical exam, except to check routine measurements such as height, weight and blood pressure.
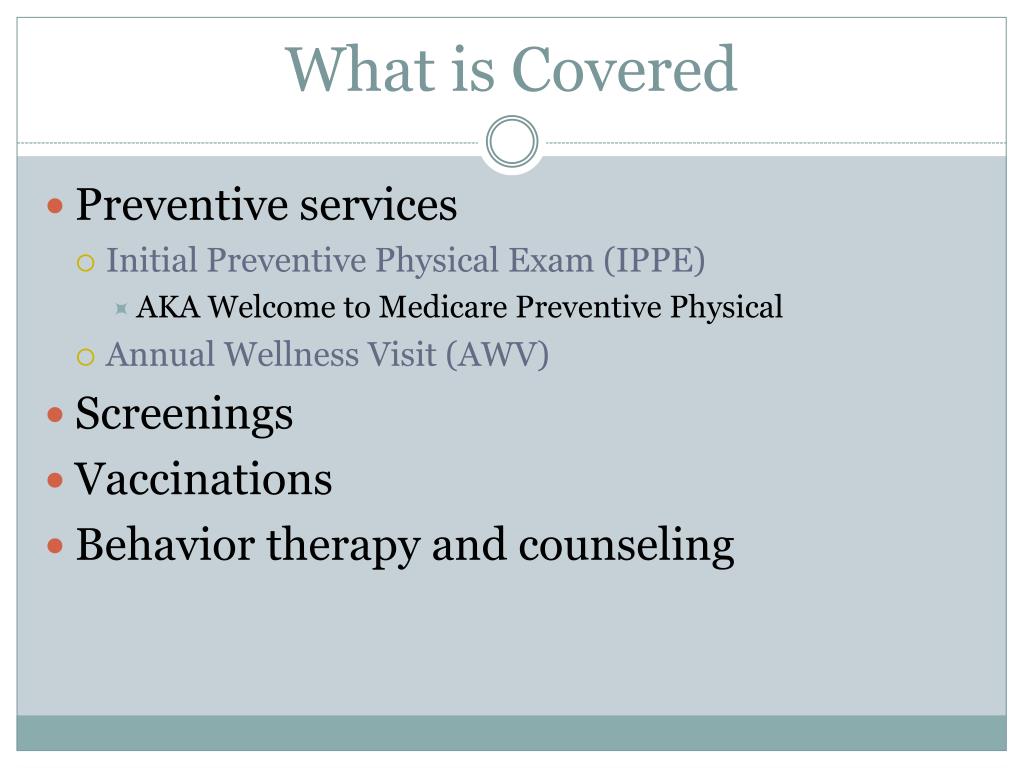
The focus of the Medicare wellness visit is on preventing disease and disability by coming up with a “personalized prevention plan” for future medical issues based on the beneficiary’s health and risk factors.
At their first wellness visit, patients will often fill out a risk-assessment questionnaire and review their family and personal medical history with their doctor, a nurse practitioner or physician assistant. The clinician will typically create a schedule for the next decade of mammograms, colonoscopies and other screenings and evaluate people for cognitive problems and depression as well as their risk of falls and other safety issues.
They may also talk about advance care planning with beneficiaries to make decisions about what type of medical treatment they want in the future if they can’t make decisions for themselves.

At subsequent annual wellness visits, the doctor and patient will review these issues and check basic measurements. Beneficiaries can also receive other covered preventive services such as flu shots at those visits without charge.
When the Medicare program was established more than 50 years ago, its purpose was to cover the diagnosis and treatment of illness and injury in older people. Preventive services were generally not covered, and routine physical checkups were explicitly excluded, along with routine foot and dental care, eyeglasses and hearing aids.
Over the years, preventive services have gradually been added to the program, and the Affordable Care Act established coverage of the annual wellness visit. Medicare beneficiaries pay nothing as long as their doctor accepts Medicare.
However, if a wellness visit veers beyond the bounds of the specific covered preventive services into diagnosis or treatment — whether at the urging of the doctor or the patient — Medicare beneficiaries will typically owe a copay or other charges. (This can be an issue when people in private plans get preventive care, too. And it can affect patients of all ages. The ACA requires insurers to provide coverage, without a copay, for a range of preventive services, including immunizations. But if a visit goes beyond prevention, the patient may encounter charges.)
And to add more confusion, Medicare beneficiaries can opt for a “Welcome to Medicare” preventive visit within the first year of joining Medicare Part B, which covers physician services.
Meanwhile, some Medicare Advantage plans cover annual physicals for their members free of charge.
Many patients want their doctor to evaluate or treat chronic conditions like diabetes or arthritis at the wellness visit, said Dr. Michael Munger, who chairs the board of the American Academy of Family Physicians. But Medicare generally won’t cover lab work, such as cholesterol screening, unless it’s tied to a specific medical condition.
Copay For Annual Physical Exam
At Munger’s practice in Overland Park, Kan., staffers routinely ask patients who come in for a wellness visit to sign an “advance beneficiary notice of noncoverage” acknowledging that they understand Medicare may not pay for some of the services they receive.
As long as beneficiaries understand the coverage rules, it’s not generally a problem, Munger said. Codes rousseau usb devices driver download for windows.
Download creamware sound cards & media devices driver. “They don’t want to come back for a separate visit, so they just understand that there may be extra charges,” he said.
Beneficiaries may not be the only ones who are unclear about what an annual wellness visit involves, said Munger. Providers may be put off if they think that it’s just another task that adds to their paperwork.
A recent study published in the journal Health Affairs found that in 2015 just over half of practices with eligible Medicare patients didn’t offer the annual wellness visit. That year, 18.8 percent of eligible beneficiaries received an annual wellness visit, the analysis found.
Primary care physicians generally want to see their patients at least once a year, Munger said, but it needn’t be for a complete physical exam.
A wellness visit or even a visit for a sprained ankle could give doctors an opportunity to check in with patients and make sure they’re on track with preventive and other care, Munger said.
Bruel & kjaer sound & vibration measurement a/s others driver download. When Dunn called the doctor’s office about the $400 bill, she said, the staff told her she had signed papers agreeing to pay whatever Medicare didn’t cover.
Dunn doesn’t dispute that.
“There were lots of papers that I signed,” she said. “But nobody told me I would get a bill for $400. I would remember that.”
In the end, the clinic waived all but $100 of the charge, but warned her that next year she’ll have to pay $300 if she wants an annual physical with that doctor. If she comes in just for an annual wellness visit, she’ll be seen by a physician assistant.
Dunn is considering her options. She would like to stay with her new doctor, who came highly recommended, and she’s worried she might have trouble finding another one just as good who accepts Medicare. But $300 seems steep to her for a checkup.
“This whole thing was so stressful for me,” she said. “I lost sleep for nights. It’s not that I couldn’t afford it, but it didn’t seem right.”
Medicare Pay For Annual Physical
Coronavirus (COVID-19) Update:
Providers are expected to refund cost-sharing amounts to beneficiaries as appropriate. |
- TRICARE Select, TRICARE Young Adult Select, TRICARE Reserve Select, and TRICARE Retired Reserve annual deductibles apply.
- TRICARE Young Adult costs are based on the sponsor's status.
- TRICARE Prime and TRICARE Young Adult Prime retirees have a separate copayment for allergy shots performed on a different day than the office visit, or performed by a different provider, such as an independent laboratory or radiology facility (even if performed on the same day as the related office visit).
- Transitional Assistance Management Program (TAMP) beneficiaries (service members and their family members) follow the active duty family member copayment/cost-share information, based on the TRICARE plan type.
A beneficiary's cost is determined by the sponsor's initial enlistment or appointment date:
Copay For Annual Physical Record
- Group A: Sponsor's enlistment or appointment date occurred prior to Jan. 1, 2018.
- Group B: Sponsor's enlistment or appointment date occurred on or after Jan. 1, 2018.
TRICARE Prime and TRICARE Prime Remote (not including TRICARE Young Adult)
| Service | Active Duty Family Members | Retirees and Their Family Members |
|---|---|---|
| Primary Care Outpatient Office Visits | Group A: $0 Group B: $0 | Group A: $21 Group B: $21 |
Specialty Care Outpatient (this includes physical, occupational | Group A: $0 Group B: $0 | Group A: $31 Group B: $31 |
TRICARE Select (not including TRICARE Young Adult)
| Service | Active Duty Family Members | Retirees and Their Family Members |
|---|---|---|
| Primary Care Outpatient Office Visits | Group A: Network Provider: $22 Group B: Network Provider: $15 | Group A: Network Provider: $30 Group B: Network Provider: $26 |
Specialty Care Outpatient (this includes physical, occupational | Group A: Network Provider: $34 Group B: Network Provider: $26 | Group A: Network Provider: $46 Group B: Network Provider: $42 |
Copay For Annual Physical Appointment
TRICARE Reserve Select (TRS) and TRICARE Retired Reserve (TRR)
| Service | TRS | TRR |
|---|---|---|
| Primary Care Outpatient Office Visits | Network Provider: $15 Non-Network Provider: 20% | Network Provider: $26 Non-Network Provider: 25% |
Specialty Care Outpatient (this includes physical, occupational | Network Provider: $26 Non-Network Provider: 20% | Network Provider: $42 Non-Network Provider: 25% |
TRICARE Young Adult (TYA)
| Service | TYA Prime | TYA Select | ||
|---|---|---|---|---|
| Active Duty Family Members | Retiree Family Members | Active Duty Family Members | Retiree Family Members | |
| Primary Care Outpatient Office Visits | $0 | $21 | Network Provider: $15 Non-Network Provider: 20% | Network Provider: $26 Non-Network Provider: 25% |
Specialty Care Outpatient Office Visits (this includes physical, | $0 | $31 | Network Provider: $26 Non-Network Provider: 20% | Network Provider: $42 Non-Network Provider: 25% |
